by Caleb Horst | Mar 20, 2020 | In The Lab
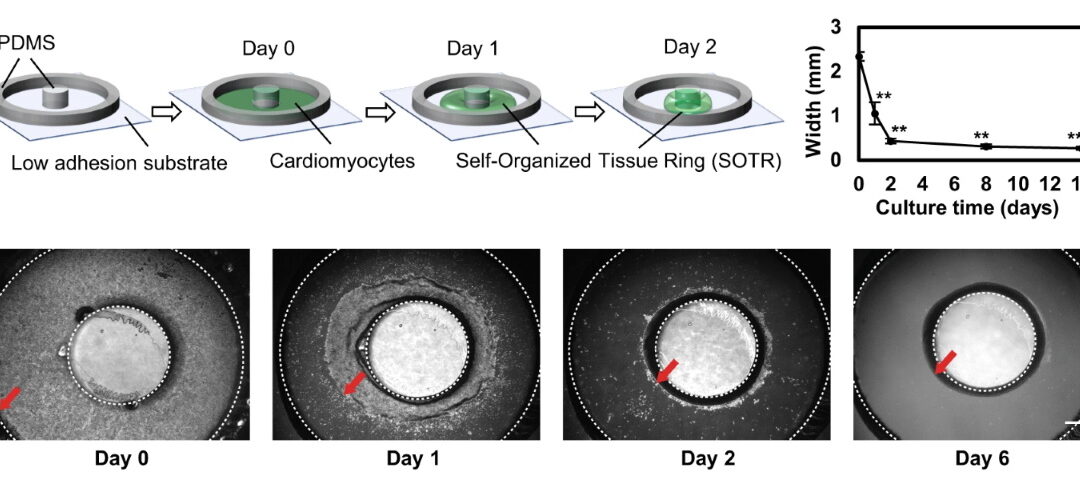
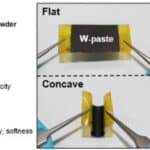
Human-induced pluripotent stem cell (hiPSC) derived cardiomyocytes present themselves as an abundant resource for tissue engineering, drug screening and regenerative-medicine applications. However, they are available in an immature state, mimicking poorly the...
by Caleb Horst | Mar 13, 2020 | In The Lab
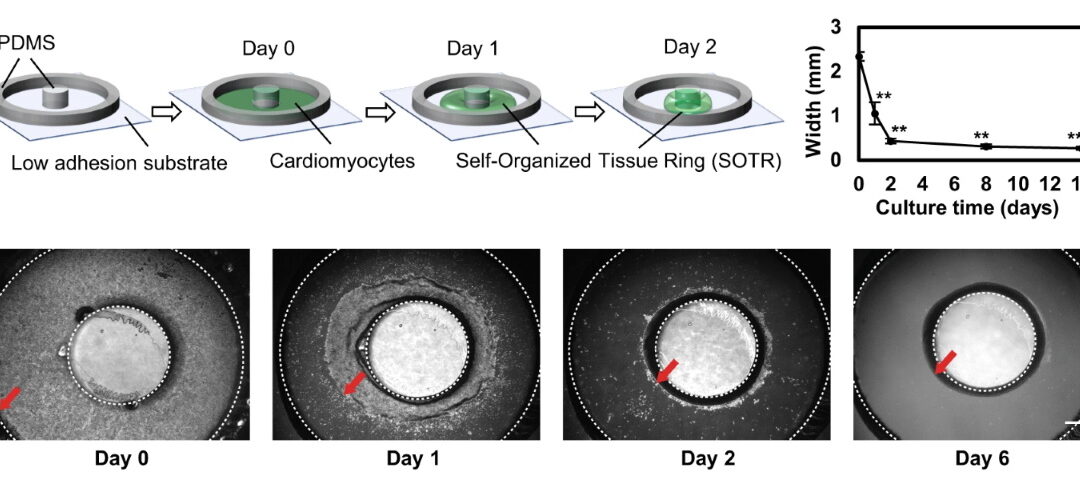
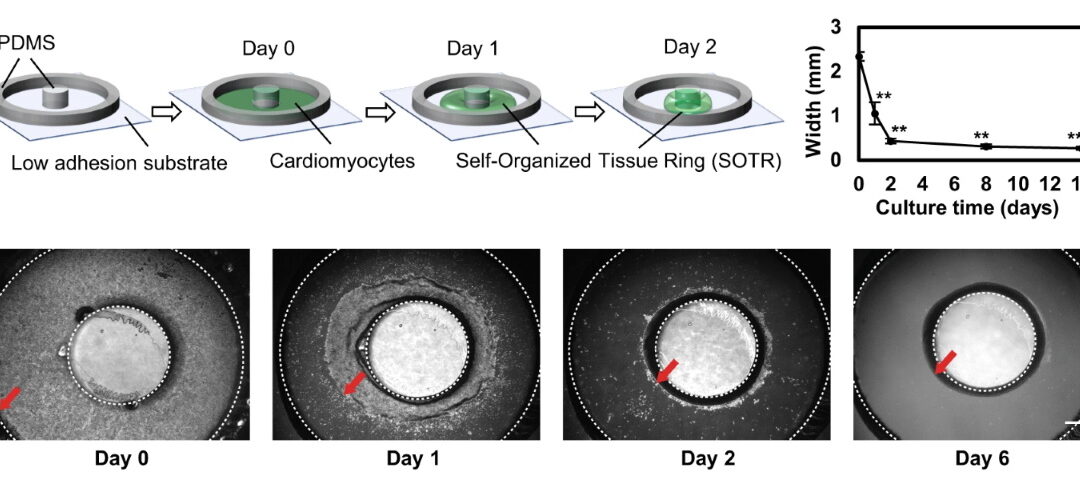
Patients with type II diabetes experience chronic wounds, a condition where wounds fail to self-heal after 3 months. Physiological processes leading to wound healing such as vascularization are disrupted and biofilms form on the wound bed that are resistant to topical...
by Caleb Horst | Feb 18, 2020 | In The Lab
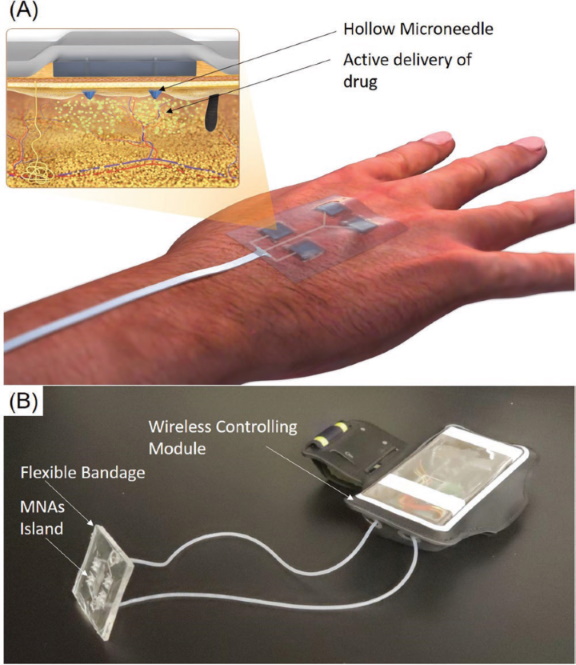
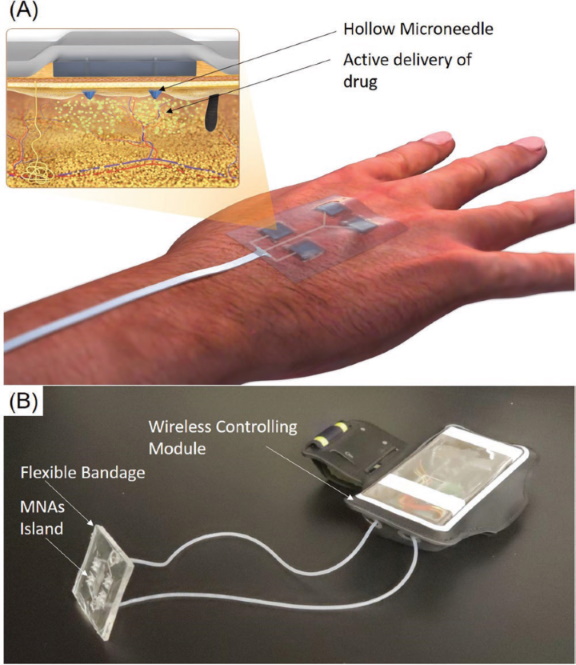
Melt processing is a manufacturing technique to create plastics with different size, shape and function. It is a continuous manufacturing process which improves the manufacturing speed and decreases costs to fabricate parts. In the biology field, components made by...
by Caleb Horst | Feb 7, 2020 | In The Lab
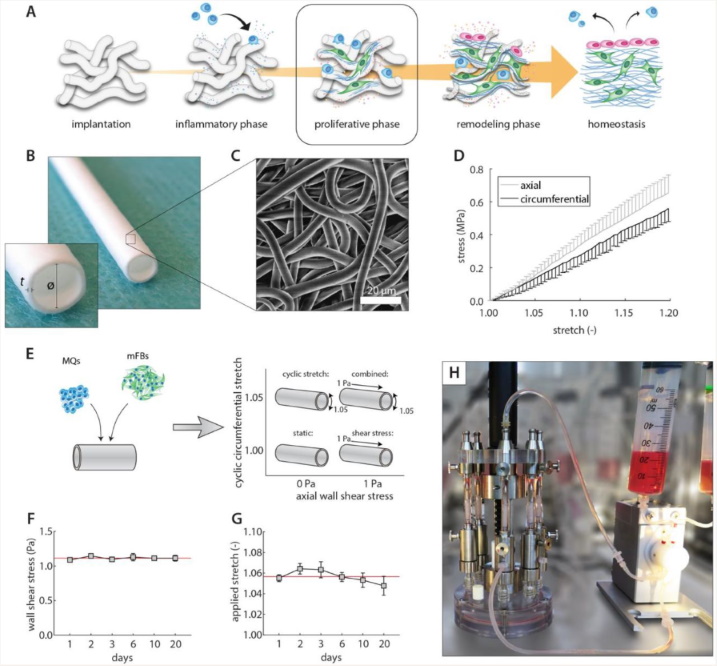
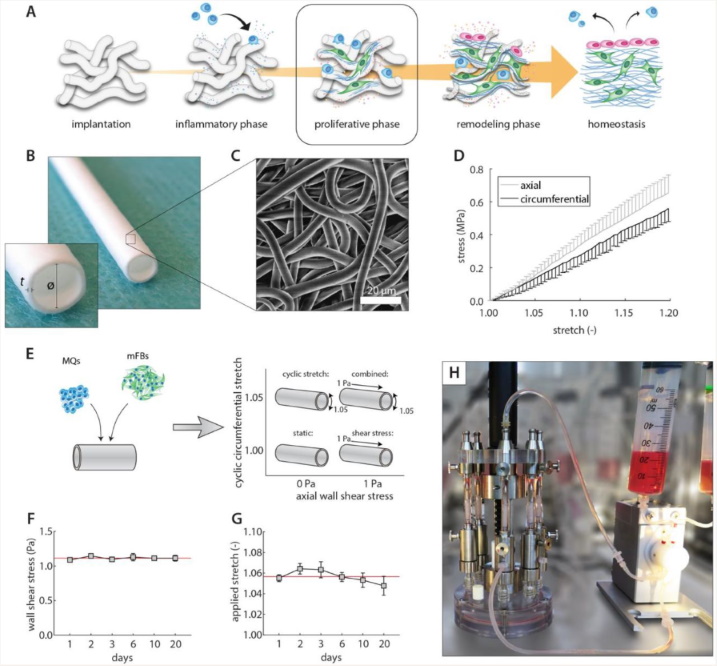
Resorbable synthetic scaffolds work to encourage tissue regeneration by allowing immune cells (e.g., macrophages) to infiltrate and attract tissue-producing cells that deposit new extracellular matrix (ECM). The deposited tissue is then remodeled to possess...
by Caleb Horst | Feb 3, 2020 | In The Lab
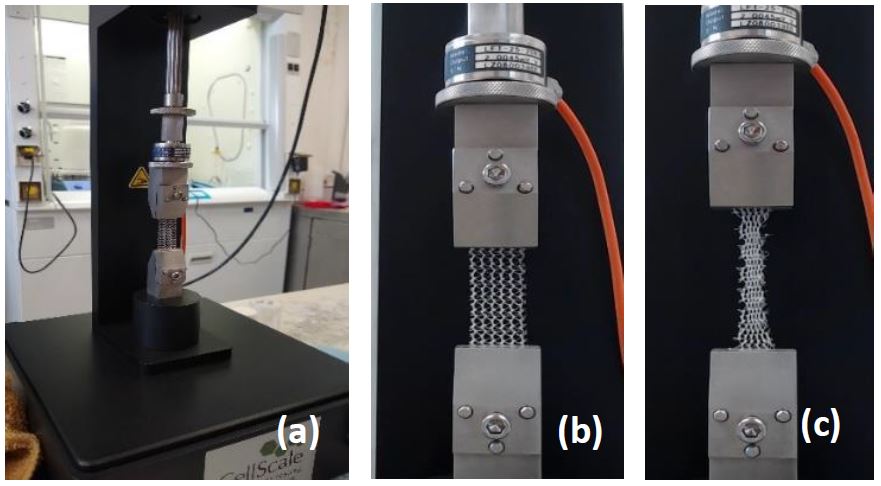
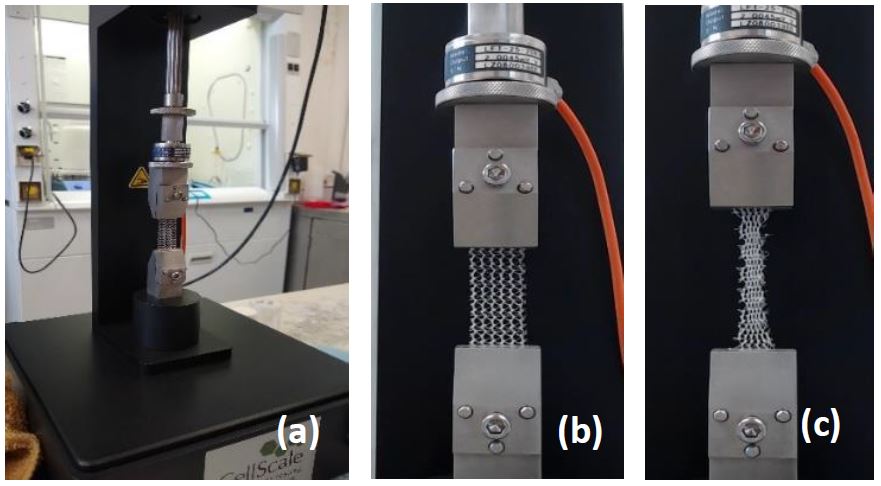
When an abdominal hernia occurs, major surgery is often required to repair it and maintain the intact lining of the abdominal sac. However, the rate of surgical failure of this procedure is high along with a hernia recurrence rate of 24-50%. Prosthetic biomaterials...
by Caleb Horst | Jan 14, 2020 | In The Lab
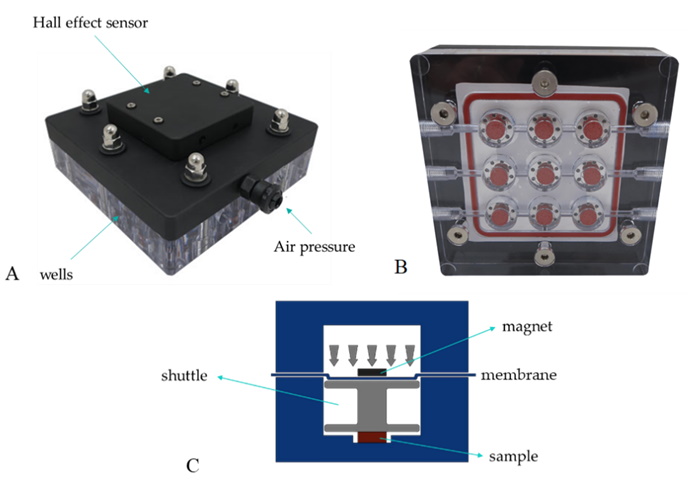
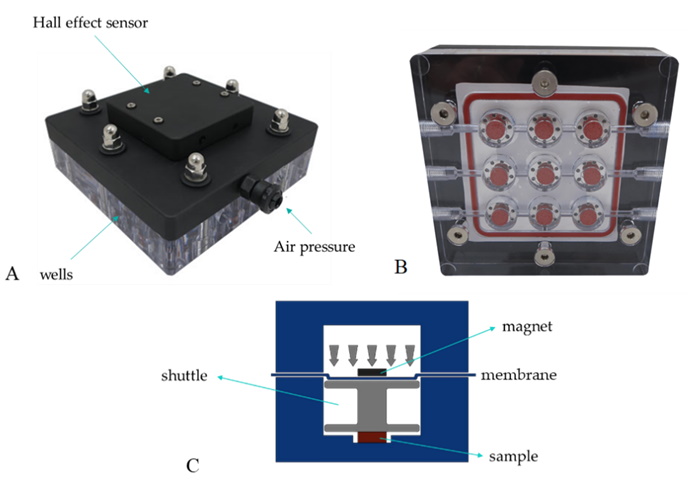
Viscoelasticity is the mechanical behavior of a material with an elastic solid phase and a viscous liquid phase, in response to an applied stimulus. Several biomaterials and biological tissues are viscoelastic and methods to measure their viscoelastic properties...